History and Development of Benzodiazepines
The History and Development of Benzodiazepines
The story of benzodiazepines began in the mid-20th century. In 1955, Polish-American chemist Leo Sternbach at Hoffmann-La Roche synthesized the first benzodiazepine while searching for a safer sedative than barbiturates. This compound, chlordiazepoxide (brand name Librium), was introduced to the market in 1960. It proved to be a breakthrough – depressant enough to calm anxiety and induce sedation, but much safer (less lethal in overdose) than the barbiturates of the 1930s–40s. Sternbach’s work laid the foundation for many benzodiazepines to follow.
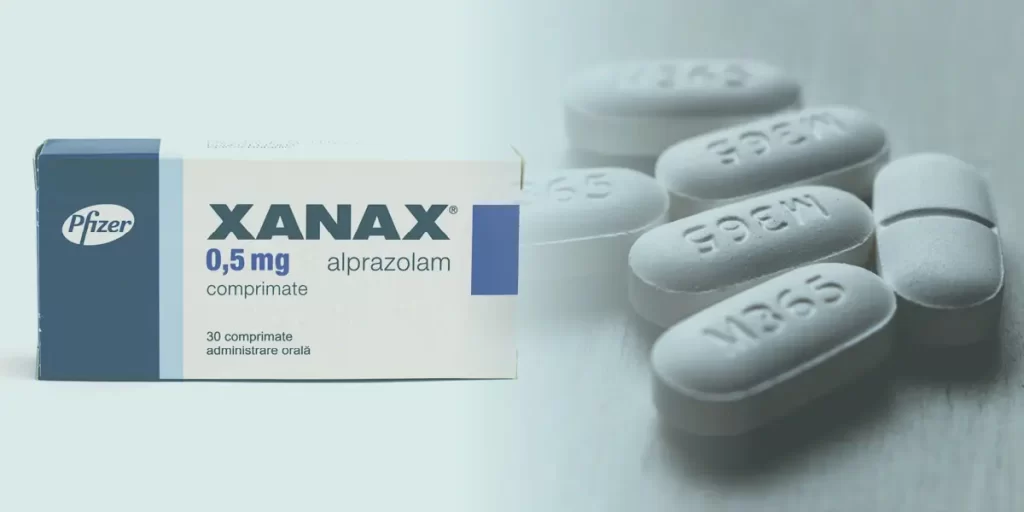
Following Librium, Hoffmann-La Roche introduced diazepam (Valium) in 1963, which rapidly became one of the best-selling drugs in the world Valium’s success led many pharmaceutical companies to develop new benzodiazepines in the 1960s and 1970s. Clonazepam (Klonopin) and lorazepam (Ativan) were marketed in 1975 and 1977, respectively, each touted as faster-acting or requiring lower dose than its predecessors. In 1981, alprazolam (Xanax) was introduced, becoming especially popular for panic disorder. Chemists often tweaked the benzodiazepine structure slightly to create these “new generation” drugs, but fundamentally they all acted on the same GABA receptors.
By the late 1970s and early 1980s, widespread use of benzodiazepines had surfaced public health concerns. Senate hearings in 1979 highlighted dependency issues, and debate grew over how to regulate them. In 1970, the U.S. Controlled Substances Act had already categorized benzodiazepines as Schedule IV drugs (lower abuse potential than Schedule II). Nonetheless, studies in the following decades confirmed that prolonged use causes tolerance and withdrawal. During the 1990s, doctors developed “Z-drugs” (e.g. zolpidem, zaleplon) as non-benzodiazepine sleep aids in hopes of reducing dependence – these target benzodiazepine receptors to induce sleep, but as noted above, they still carry similar risks.
In recent years, medical agencies have acted on lessons learned. Starting in 2015, the U.S. FDA mandated stronger labeling for benzodiazepines, and by 2020 boxed warnings were required on all products to highlight the risks of misuse, dependence, and overdose. Today, benzodiazepines remain valuable for short-term symptom control, but they are prescribed far more cautiously. Guidelines strongly recommend these drugs only for brief periods, and healthcare providers emphasize patient education on tapering and alternatives. Wolfman Pharmacia acknowledges this history by balancing our offering of these medications with clear information and support, ensuring patients use benzodiazepines as they were intended – safely and responsibly.